Researchers in Europe have developed a way to vaccinate mice against Alzheimer’s disease, an approach they hope could one day be successful in people.
The work is the latest attempt to target amyloid beta proteins, which are thought to play a central role in the development of the disease.
Scientists hope to undertake clinical trials, although experts have given a warning that success against Alzheimer’s in animals often does not translate into results with human beings.
Many attempts to develop treatments focus on amyloid beta aggregates, or plaques, that build up in the brains of people with the condition.
The research from the University Medical Centre Goettingen in Germany, the University of Leicester in the UK and LifeArc, a British medical research charity, instead involves a truncated, soluble form of the protein found in some fluids in the body.
This form is thought to be linked to the damage to nerve cells in the brain that is associated with Alzheimer’s disease.
LifeArc
The researchers identified a mouse antibody that neutralises this truncated amyloid beta protein but does not target normal “string-like” forms of the protein or the amyloid beta plaques.
To reduce the likelihood of an immune response in people, LifeArc developed what it described as a humanised version of the antibody called TAP01_04.
When analysing how this antibody binds to the truncated amyloid beta, the researchers in Leicester found that the protein was folded back on itself like a hairpin.
They generated a stable fragment of this protein region, which could be used in a vaccine to make a person’s immune system generate antibodies like TAP01_04 and protect against the disease.
When this engineered protein was tested on mice by the Leicester researchers, the creatures’ immune systems produced antibodies.
The humanised antibody and the engineered amyloid beta vaccine, called TAPAS, was then tested by the researchers in Germany on mice with Alzheimer’s.
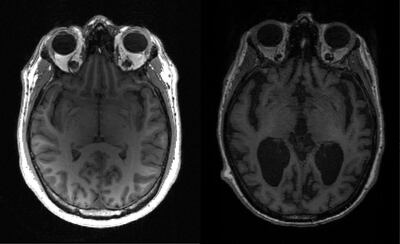
Imaging techniques found the vaccine and the antibody restored the function of nerve cells, increased glucose metabolism in the brain, restored memory loss and reduced the formation of amyloid beta plaques.
“The TAP01_04 humanised antibody and the TAPAS vaccine are very different to previous antibodies or vaccines for Alzheimer’s disease that have been tested in clinical trials, because they target a different form of the amyloid beta protein,” said Dr Preeti Bakrania, a LifeArc scientist.
“The results so far are very exciting and testament to the scientific expertise of the team. If this new approach proves successful, it could transform the lives of many patients.”
The scientists would like to find a commercial partner to fund clinical trials of the therapeutic antibody and the vaccine.
Concerns over effectiveness
Alzheimer’s causes about two thirds of cases of dementia in the over-65 age group and affects more than 44 million people worldwide, although numbers are expected to double every two decades, according to Alzheimer’s Disease International.
The course of the disease typically lasts about 25 years, but this includes a substantial period before symptoms materialise, such as memory loss and speech problems.
The new approach could be used to treat Alzheimer’s once symptoms are displayed and to produce a vaccine to be used before the appearance of symptoms.
Prof Paul Morgan, of the UK Dementia Research Institute at Cardiff University, said that while the research was interesting, it may not represent a breakthrough, because work targeting amyloid had been going on “for decades”.
“There have been many approaches targeting amyloid and different forms of amyloid, from aggregate to more soluble forms,” he said.
“Often they show some success in preclinical [research] but often, if they get to the clinic, they don’t seem to have the same degree of effect. At the moment, I don’t think the evidence is there that this is a game-changer.
“We need to be doing lots of different things, trying new approaches, looking for things other than amyloid.”
The findings, published in Molecular Psychiatry, come five months after the approval of the first therapy that could actually slow the progression of Alzheimer’s disease instead of merely treating its symptoms.
The approval of aducanumab in June was divisive because some scientists and organisations felt that clinical trials had not yielded convincing evidence that the drug was effective.
Work so far targeting insoluble forms of amyloid proteins using antibodies has failed, so focusing on soluble forms is unlikely to succeed either, said David Smith, professor emeritus of pharmacology at the University of Oxford.
“I don’t think there will ever be a cure for Alzheimer’s itself,” Prof Smith said. “Once it’s been diagnosed, the brain is too far gone. You’re not going to be able to rebuild the lost memories.”
Prevention is a better approach, he said, drawing comparison with efforts to combat heart disease, which have saved thousands of lives by identifying and treating risk factors such as high blood pressure. Epidemiological research can try to identify risk factors for Alzheimer’s, he said.


