Women from the Gulf are at higher risk of endometrial cancer but new breakthroughs in genetic testing of the disease mean more lives will be saved, a doctor from London’s specialist cancer hospital has told The National.
Endometrial cancer affects the lining of the womb and cases of the disease have doubled in the past 10 years in western countries.
For patients from the Gulf, this could be even higher. “We’ve seen a huge increase in women from the Gulf coming to the UK for consideration for treatment,” said Dr Angela George, a consultant oncologist at The Royal Marsden Hospital, who has been leading research to identify genes that cause the disease.
Dr George believes the cancer is endemic in the Gulf, even though statistics on patient numbers are not yet available. “In almost every family in the Gulf, there will be women who have endometrial cancer right now,” she estimated.
Conditions such as diabetes and obesity may be responsible for this increase, as well as a drop in the number of women having their wombs surgically removed after they have completed their families. “Twenty or 30 years ago, it wasn’t uncommon for women to have their wombs removed when they reached their 40s and 50s,” said Dr George.
Yet survival rates globally have not improved as much as in other areas of cancer in the past decade, due to a “neglect” of the condition. “For many years there was little interest in doing research on it, there weren’t any exciting new drugs,” Dr George said.
But this may change as new forms of diagnosis – known to doctors as genomic or molecular profiling – allow them to better tailor the treatment to the patient and identify those at risk before they develop the disease.
These tests for full molecular profiling became routinely available on Britain’s National Health Service at the end of last year, and are also available privately. “Molecular profiling has led to a whole new era of molecularly matched treatments for patients," said Dr George. "It’s gratifying to see that these patients, who were a really neglected group for a long time, are finally doing well and finally having long-term survival."
Why is molecular profiling used in cancer care?
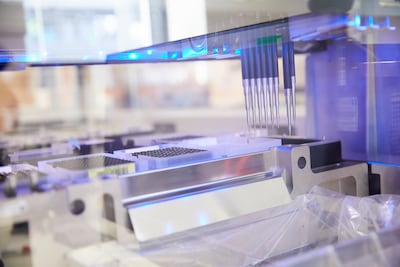
Molecular profiling examines the gene alterations of a patient’s tumour to help identify the best course of treatment. “It informs you how the tumour is going to behave, what treatments are most likely to be successful for them and whether it's likely to return in the future or not,” she explained.
A piece of a patient’s tumour is removed and examined. “Ideally this is done when they have their first tumour biopsy that confirms they have a cancer in the first place,” she said. But it could also be done after a cancer has been diagnosed and the tumour itself is removed.
Gene alterations from these tests allow oncologists to separate women into four different “molecular” groups. “One group does extraordinarily well, one does OK if you give them the right treatment and a third group will have a slow but well-behaving cancer.” she explained. “The fourth group will have a very, very aggressive disease that is very likely to return in the future.”
Each of these groups will respond to different types of treatment. “Two of these groups do very well with immunotherapy. One does well with chemotherapy and one does well with hormone treatment,” Dr George said.
“You can make sure that you're giving the patient the treatment they are most likely to respond to and avoid unnecessary side effects."
The method has proven effective in identifying women at high risk of an aggressive, recurring cancer at early stages of the disease. “Previously, they may not have been offered treatment," said Dr George. "But we now know on the basis of the changes in their tumour that they are high-risk patients and they need additional treatment."
Results were already visible from clinical trials. “We’re not seeing the relapses in the patients that we would expect: patients with advanced disease or high-risk disease,” said Dr George. The trials took place over seven years and were supported by Royal Marsden Cancer Charity with funding from the Lady Garden Foundation.
Dr George hopes survival rates for endometrial cancer will rise within the next five years. “Now that we have the options available to us, and now that we can select the appropriate treatment for patients, we expect to see much better outcomes,” she said.
Helping families know who is at risk
Molecular profiling will reduce the risk of patients developing endometrial cancer in the first place, by identifying those who carry the cancer-causing gene alteration.
One in 10 women with endometrial cancer had an inherited gene alteration that caused the disease, Dr George found during her research. “I identified quite a lot of these women from the Gulf among them,” she added.
About 30 per cent of patients will have changes in their tumour who require ongoing testing for an inherited gene alteration. Of these, a third will have a gene alteration and, as such, are at risk of developing other specific cancers, including of the bowel.
Men could also be carriers and the condition puts them at high risk of colorectal, bowel, stomach and urinary tract cancer, among others.
Understanding these genetic factors can also help identify relatives who may be carriers. “The patient’s brothers, sisters and children have a 50 per cent chance of carrying the same gene alteration,” said Dr George.
Family members can get tested for these alterations through blood tests at a genetics clinic. “I look after a lot of families who have been picked up while they were over here [for a relative’s] treatment. We’ve been able to make recommendations for the wider family,” she said.
Once the gene alteration has been pinpointed, a patient can take simple preventive measures which would lower their risks of developing the cancer. These are as simple as taking a baby aspirin every day, which would halve the risk of getting any of the related cancers in the future.
The research team's latest findings on molecular profiling for endometrial cancer will be presented in the coming months, as more clinical trials are being set up. Dr George said: “We’ve identified a number of other molecular factors, which are treatable with patients whose disease returns, that we're looking at setting up clinical trials for."


